41 – So what’s this Immunotherapy all about?
23 December 2022
They say one shouldn’t spend too much time on the internet trying to find out about cancer treatments. And on the whole, I’d say that’s pretty good advice.
Unless you’re Wozzer that is!
Unfortunately, I have too much time on my hands these days, so checking stuff on the web is right up my street.
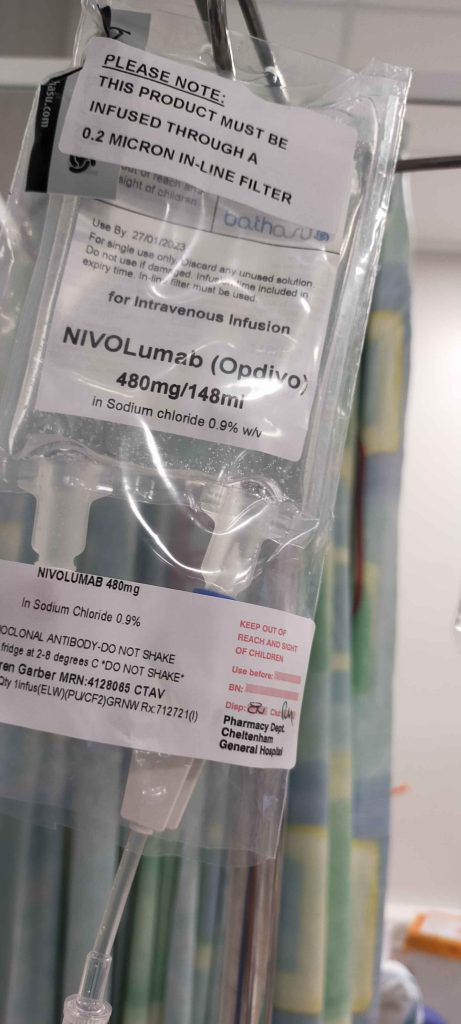
And when Dr Grant discussed my new immunotherapy treatment, with a drug named Nivolumab (brand name Opdivo), of course I had to check it out on Wikipedia: https://en.wikipedia.org/wiki/Nivolumab
I’ll admit to not understanding most of what’s written, but one line certainly grabbed my attention:

‘It is made using Chinese hamster ovary cells’. Blimey! Really?
Of course, I’ll roll with it – if Dr Grant says it’s fine, that’s good enough for me.
Immunotherapy is completely different to the more well-known Chemotherapy. The key difference is in the way that they ‘target’ cancer cells.
Here’s my simple understanding:
Our bodies are comprised of literally billions of cells, that provide the complete structure of how we are and how we live eg, nerve cells, blood cells, muscle cells and more. They’re all working 24/7 and can repair themselves if things are going wrong (viruses etc). They can die and duplicate so that new cells replace the dead ones.
Sometimes though, in some people – cell structures can become damaged inside and they start to duplicate uncontrollably, growing as cancerous tumours.
And even worse, they can spread to other parts of the body and begin to grow and develop in or on other organs, known as ‘metastasis’.
And if those two statements are not bad enough, the ‘metastatic’ cancer cells can send signals to our body’s own immune system (antibodies) to stop trying to fight or ‘cure’ them. Which is what makes cancer so scary, because by this step – the cancer is usually incurable.
So, Chemotherapy attempts to reduce the uncontrollable cell-splitting duplications, but unfortunately can and does stop healthy cells from duplicating too. This is why there are generally such severe side-effects associated with this type of treatment.
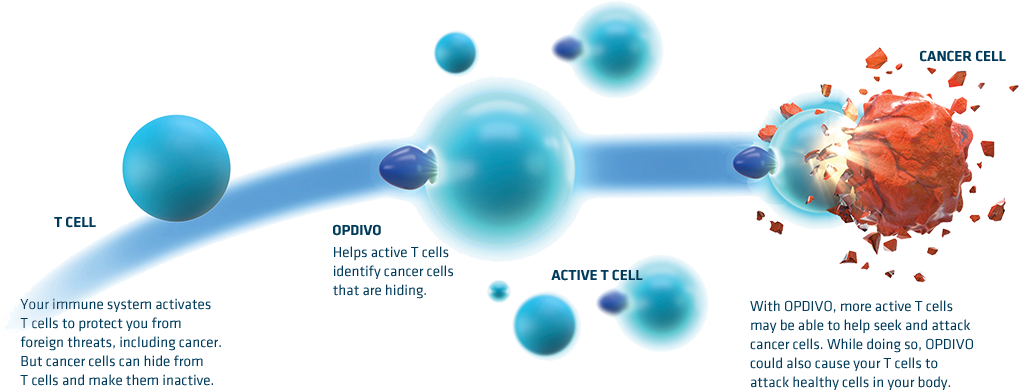
Immunotherapy takes a more subtle and technical approach. It trains / stimulates (or boosts) our own immune system to ignore the ‘I’m friendly’ signals from cancer cells and to attack those cells in any case.
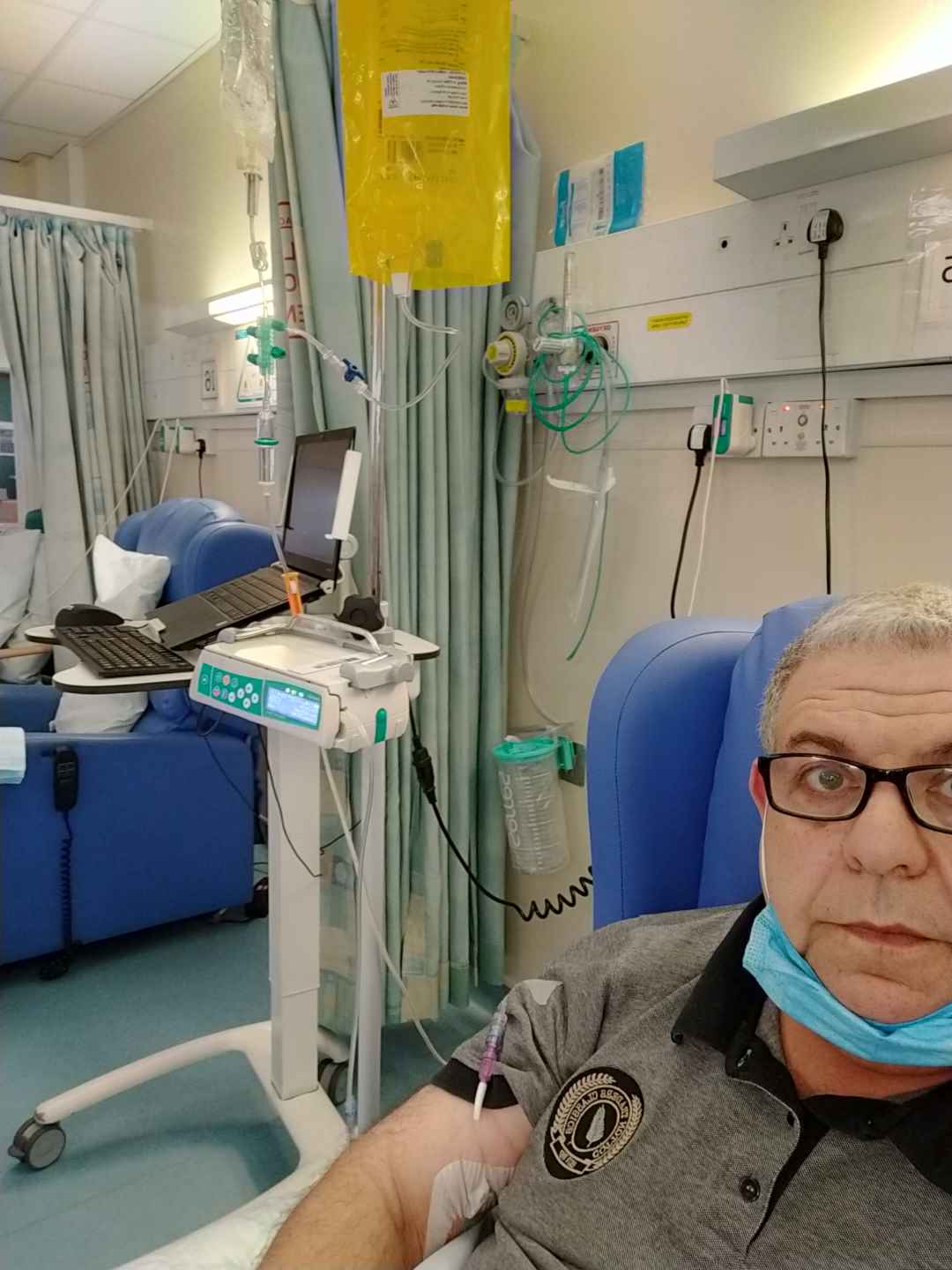
To date, I’ve just finished my 3rd infusion of Nivolumab and now have one just one treatment per month by IV. It takes around one hour to infuse.
So far so good. I’ve haven’t had any obvious side-effects and hopefully will have another CT scan in January, so that we can get some kind of indication as to whether it’s working, or not.
But I can’t seem to get the thought of the Chinese hamster out of my mind – and how much of it is now inside me!
So if anyone sees me nibbling on cheese – or even worse running on a wheel – for goodness sake, please contact Cheltenham Oncology Centre on my behalf 😉
More from me in a month or so, but until then Wozzer wishes you all – wherever you are in the world, a very merry Xmas and a happy, prosperous and healthy New Year!
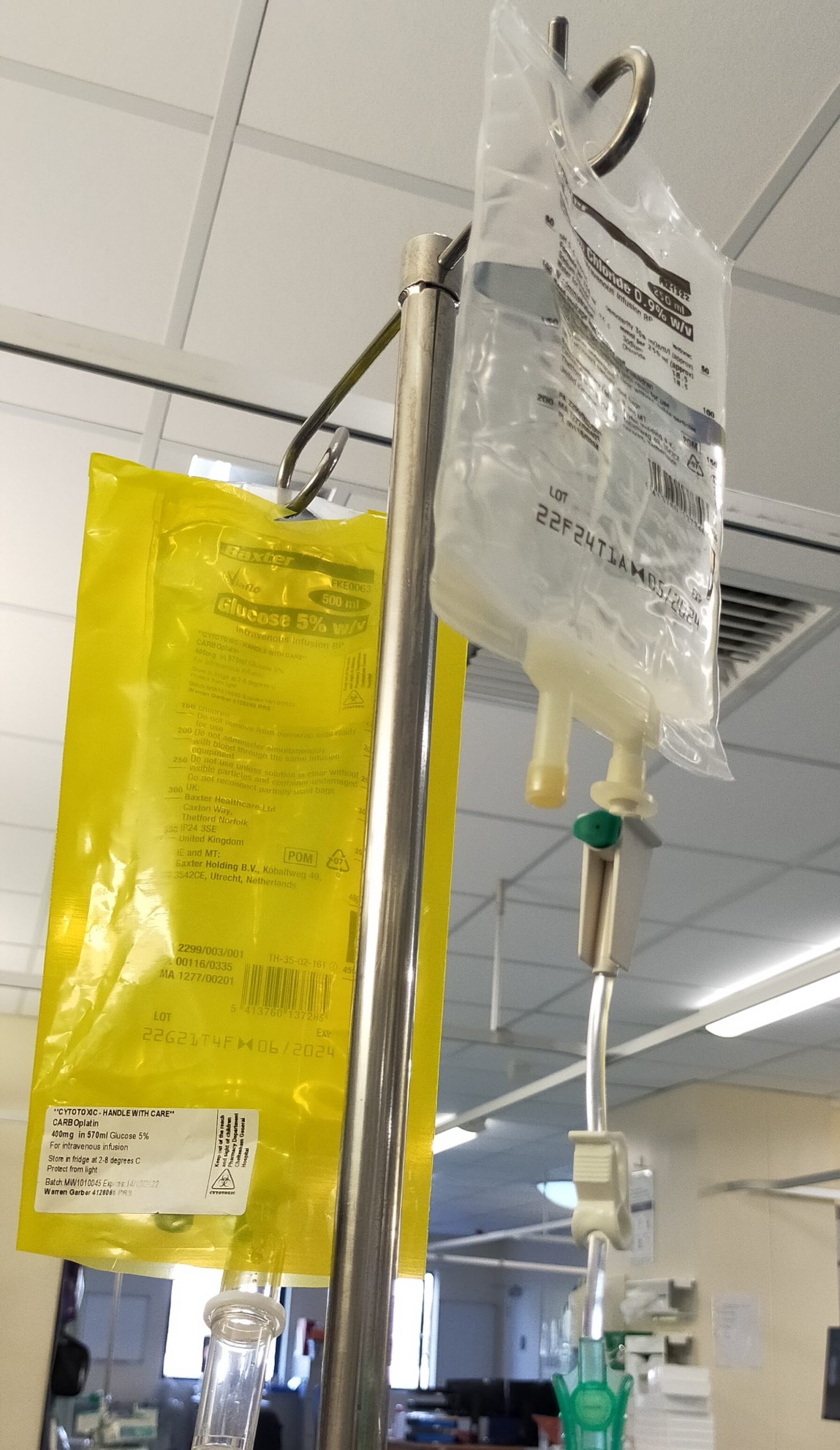

















 This is followed up by a good shot of Dexamethasone, which is a steroid. It’s used for many treatments, but in my case to help the body transition with the chemotherapy drugs. After that I get a dose of an anti-sickness medication and then finally hooked up to the Carboplatin chemo. This infusion takes around an hour.
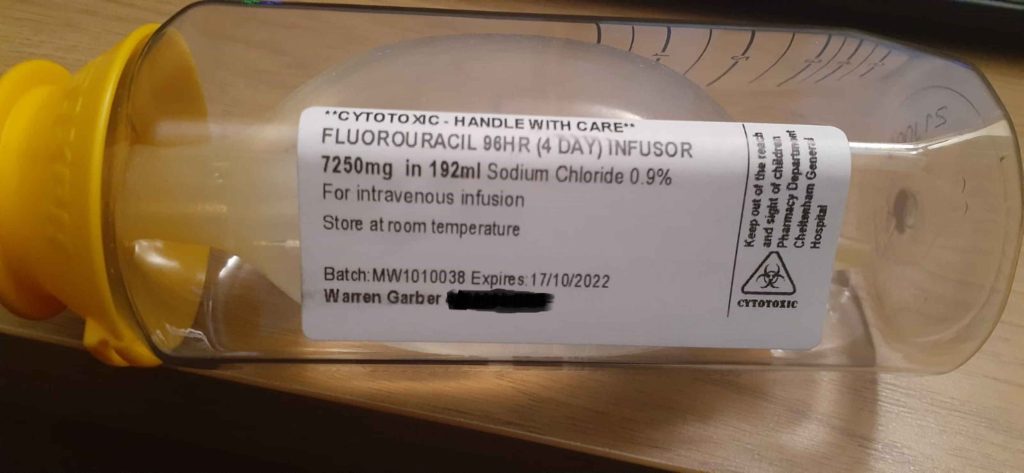
This is followed up by a good shot of Dexamethasone, which is a steroid. It’s used for many treatments, but in my case to help the body transition with the chemotherapy drugs. After that I get a dose of an anti-sickness medication and then finally hooked up to the Carboplatin chemo. This infusion takes around an hour.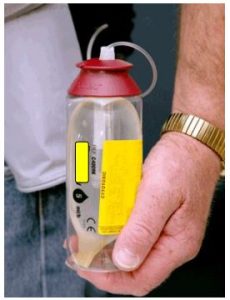 Kat puts it all together and places the Infusor into a small ‘bum bag’, which attaches to my belt. That’s me and the Infusor ‘married’ for a few days. I can’t disconnect it and must get used to it being there – including while sleeping, without of course, allowing the line to become tangled or disconnected.
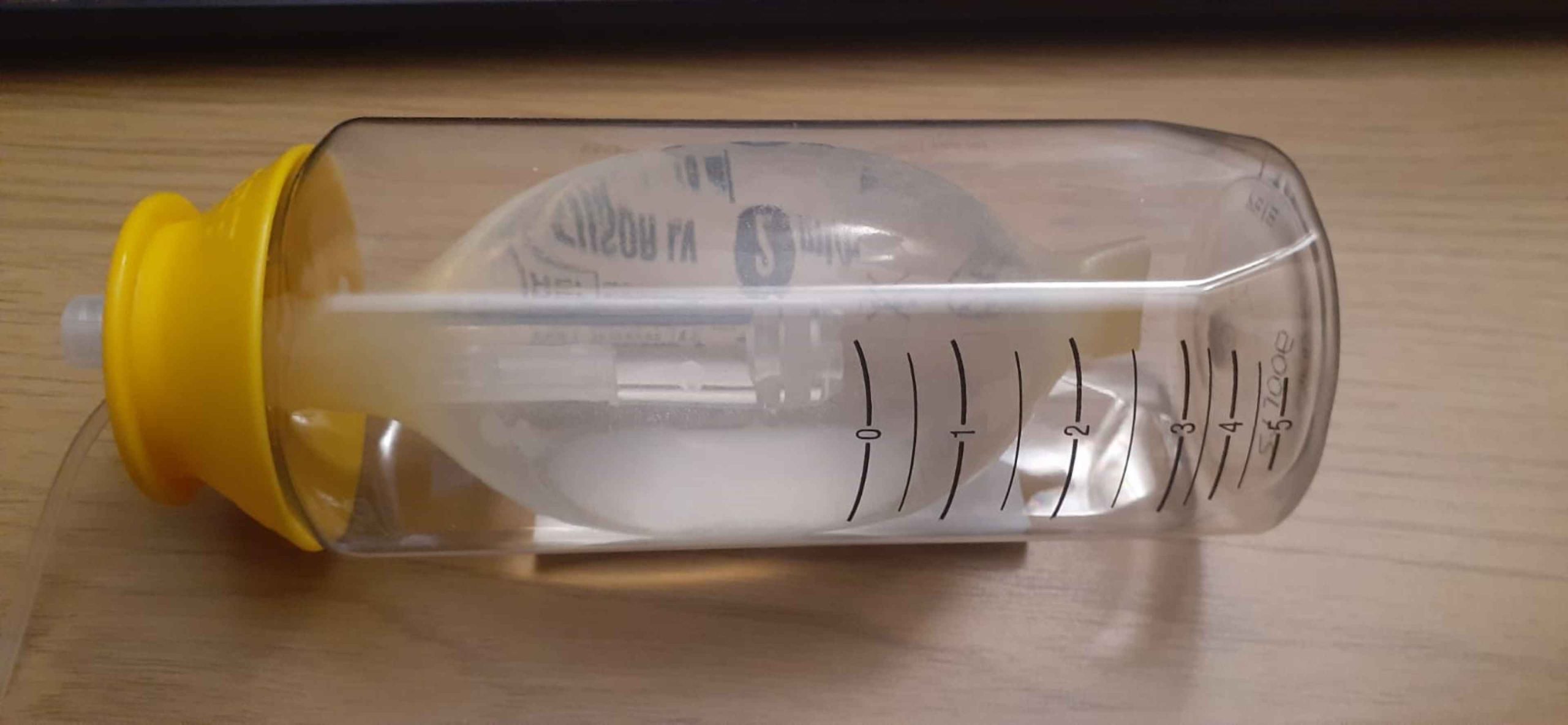
Kat puts it all together and places the Infusor into a small ‘bum bag’, which attaches to my belt. That’s me and the Infusor ‘married’ for a few days. I can’t disconnect it and must get used to it being there – including while sleeping, without of course, allowing the line to become tangled or disconnected. It’s pretty amazing how we adapt to new things. In 60 odd years, I’ve never slept on my back – but immediately I find that wedging the Infuser behind my pillows, gives me enough play in the line that I can (almost) sleep comfortably.
It’s pretty amazing how we adapt to new things. In 60 odd years, I’ve never slept on my back – but immediately I find that wedging the Infuser behind my pillows, gives me enough play in the line that I can (almost) sleep comfortably.