45 – Palliative Care – a term with an unfortunate reputation
12th July 2023
‘Hello Warren – this is the Palliative Care Team at Gloucester Royal Hospital. We’d like to make an appointment to visit you.’
So, there’s a term almost guaranteed to strike fear – or at the very least an awful feeling of unease into oneself.
And why?
Because many of us confuse ‘Palliative Care’ with ’End of Life’ care.
While many think palliative nurses (for instance) are just there to administer a good ol’ dose of morphine (or whatever), to relieve the worst of pain, right at the end of life – the actuality is far from that.
Within the cancer treatment world, there are a couple of key conditions and a couple of treatment regimes. These are curable or incurable cancer and curative treatments or palliative treatments.
Sure, I’m oversimplifying the broad spectrum of all possible treatment regimes, but to illustrate this article, hopefully this will do:
In my case, back in April 2020 I was diagnosed with throat cancer and as it was considered curable, I was given curative radiotherapy over six weeks. For many people, that should be it – and with regular checks for 5 years or more,they might not see any return of the cancer.
For those not so lucky - like me, where the cancer subsequently spread to other parts of the body, this is termed ‘metastatic cancer' and for a lot ofcomplex biological reasons, the cancer becomes incurable. My spread to the right lung was first noted by CT scan in September 2020.
So – for the best part of 3 years I’ve been living with incurable cancer. Therefore the treatments I’ve received during this time (Chemotherapy, Radiotherapy and Immunotherapy) have all been termed palliative treatments.
A definition of Palliative Treatment:
a medicine or form of medical care that relieves symptoms without dealing with the cause of the condition.
This has all been brought to the forefront of my life, because I received the first contact from my palliative care team at my local hospital recently.
Believe me, I felt like it was a phone call from the grim reaper himself ☹
But of course, it was nothing like that. We discussed all kinds of things from counselling, through finances, daily living, medications and medical aids or equipment that might be required – now or in the future.
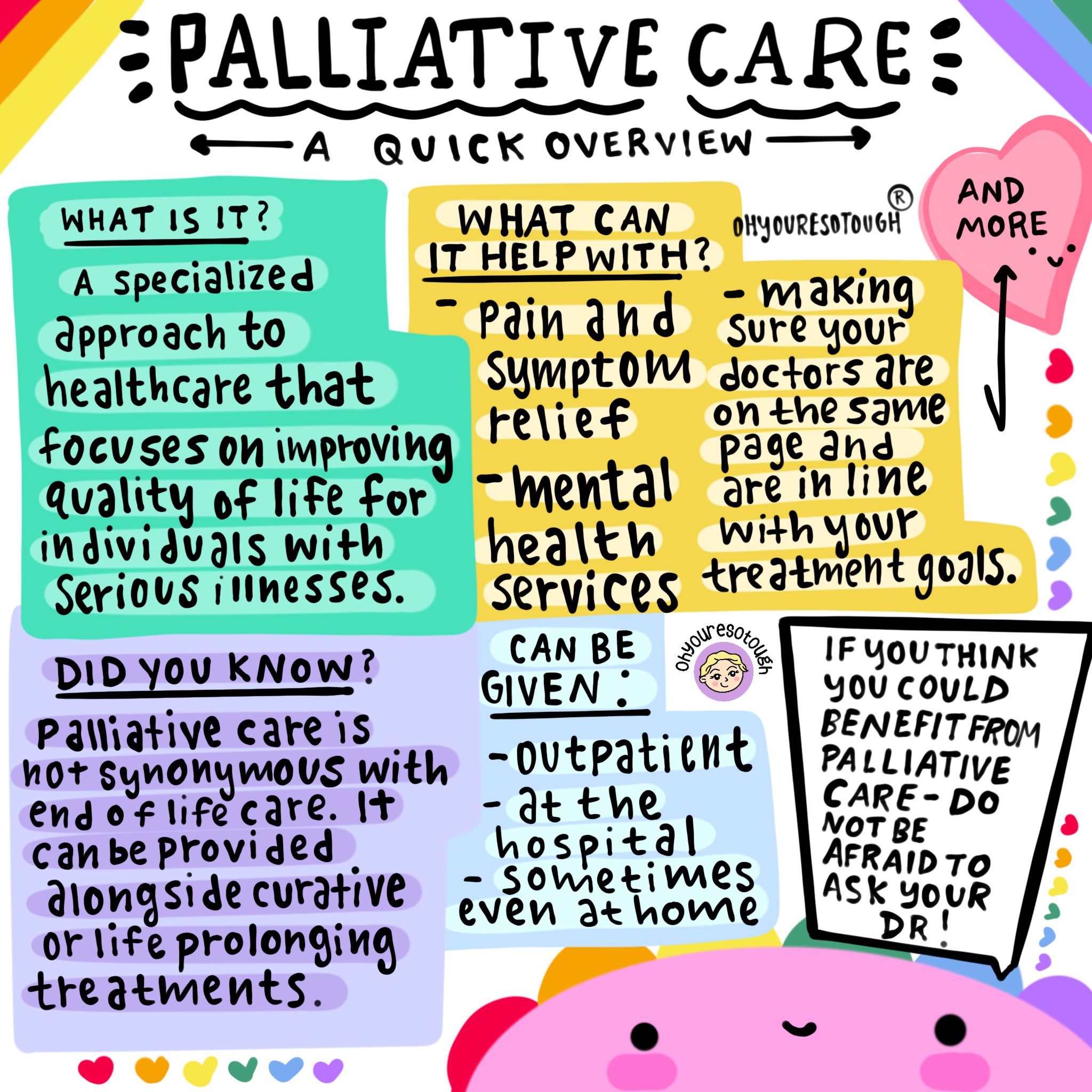
I did come by a great infographic by a contact of mine on Twitter (yes, I know - as if I’m not sick enough as it is). It explains clearly what I’ve been waffling on about – and hopefully will help anyone who, for whatever reason, finds themselves in the realms of receiving, or explaining Palliative Care to relatives or friends.
Chelsey Gomez is an artist and cancer survivor. She creates art to help and inform other cancer patients of all ages. Never spoken to her, just messaged a few times, but I love her work.
Chelsey has kindly given me permission to add her Palliative Care artwork into my blog and by clicking on it, will open her website (in a new tab).
So yes, there will come a time for the Palliative Nurse Team to be here for my 'end of life' treatment and care - but I'm not booking them in for any time soon 🙂








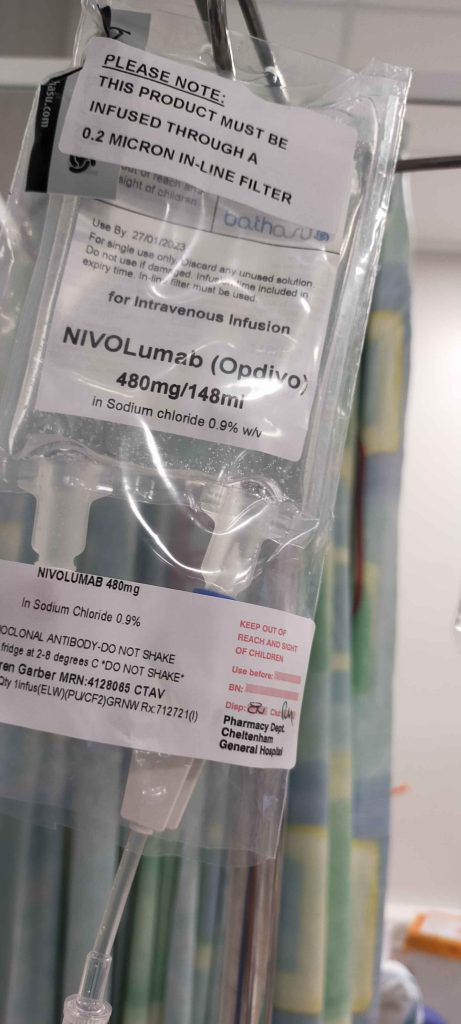
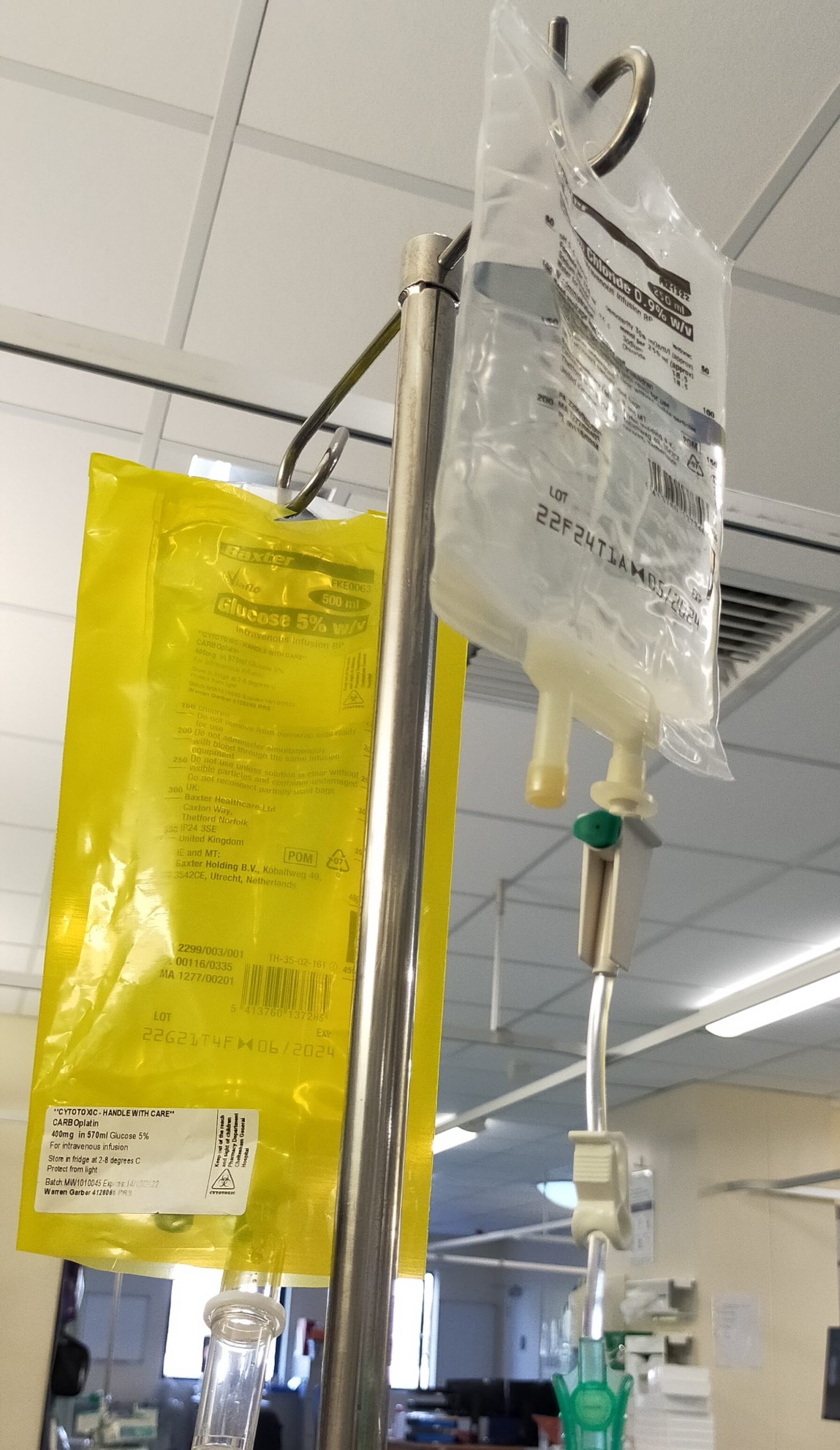






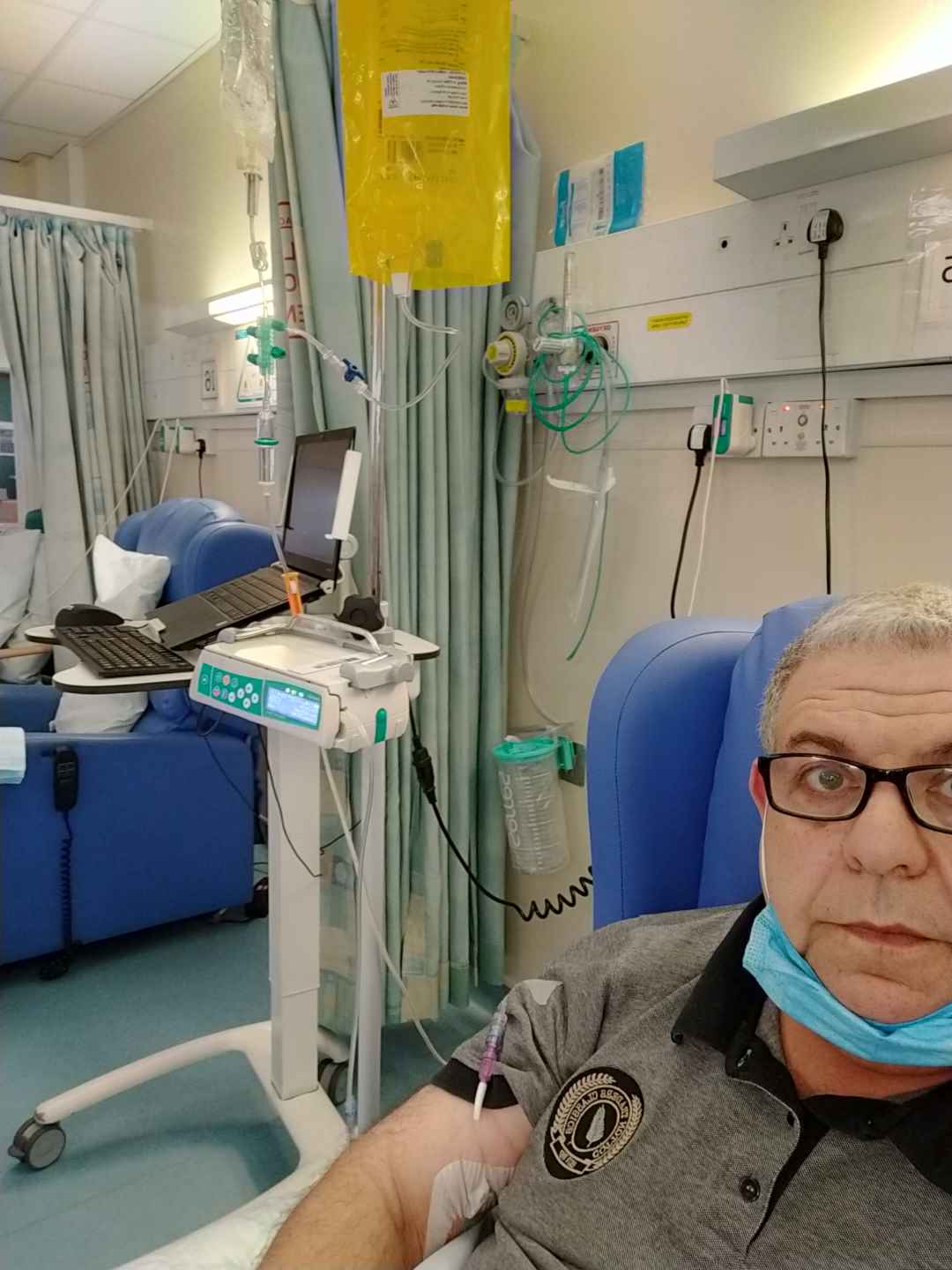
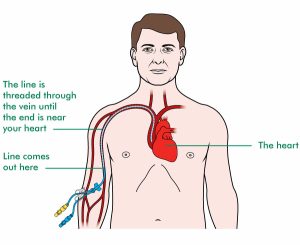
 This is followed up by a good shot of Dexamethasone, which is a steroid. It’s used for many treatments, but in my case to help the body transition with the chemotherapy drugs. After that I get a dose of an anti-sickness medication and then finally hooked up to the Carboplatin chemo. This infusion takes around an hour.
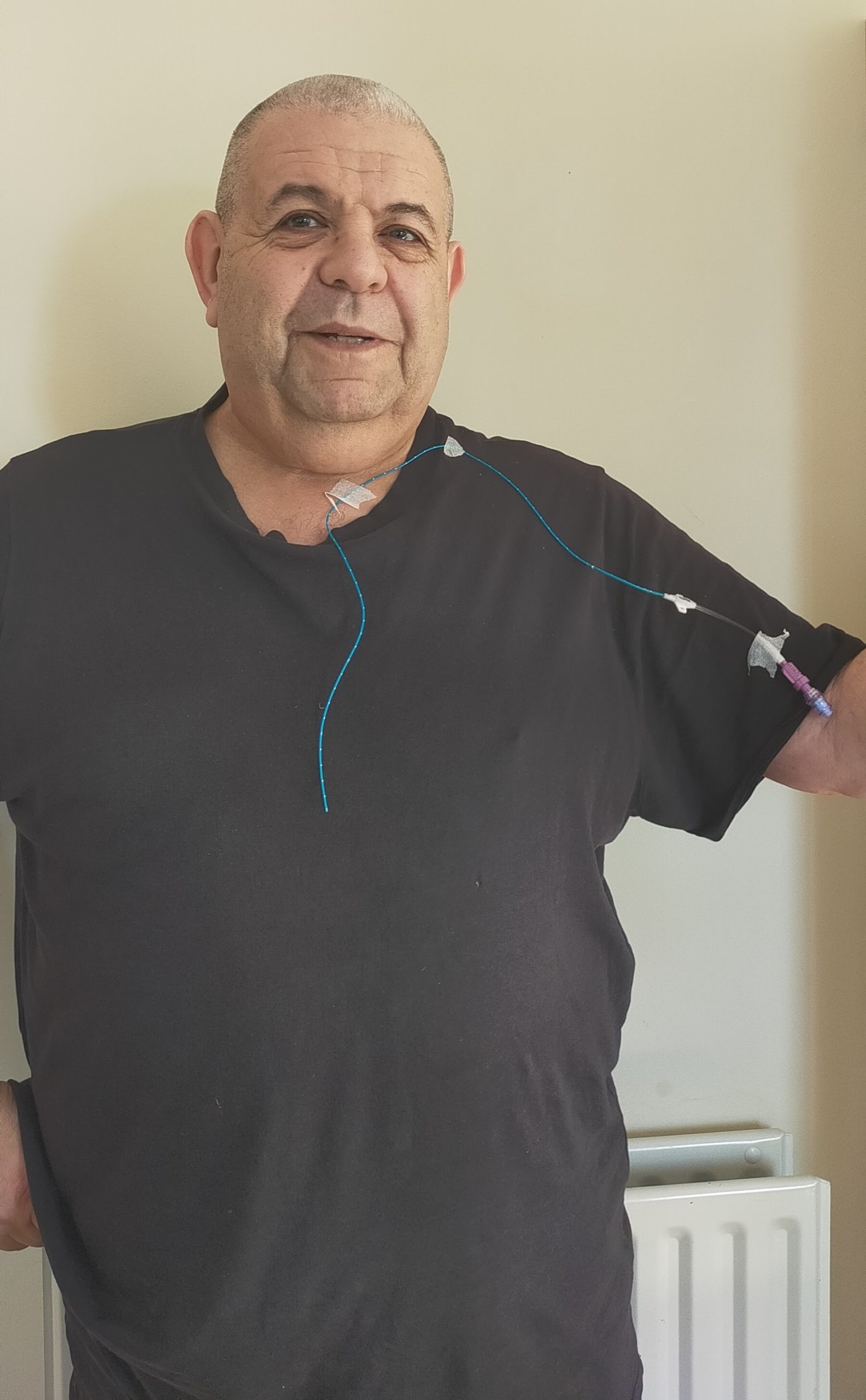
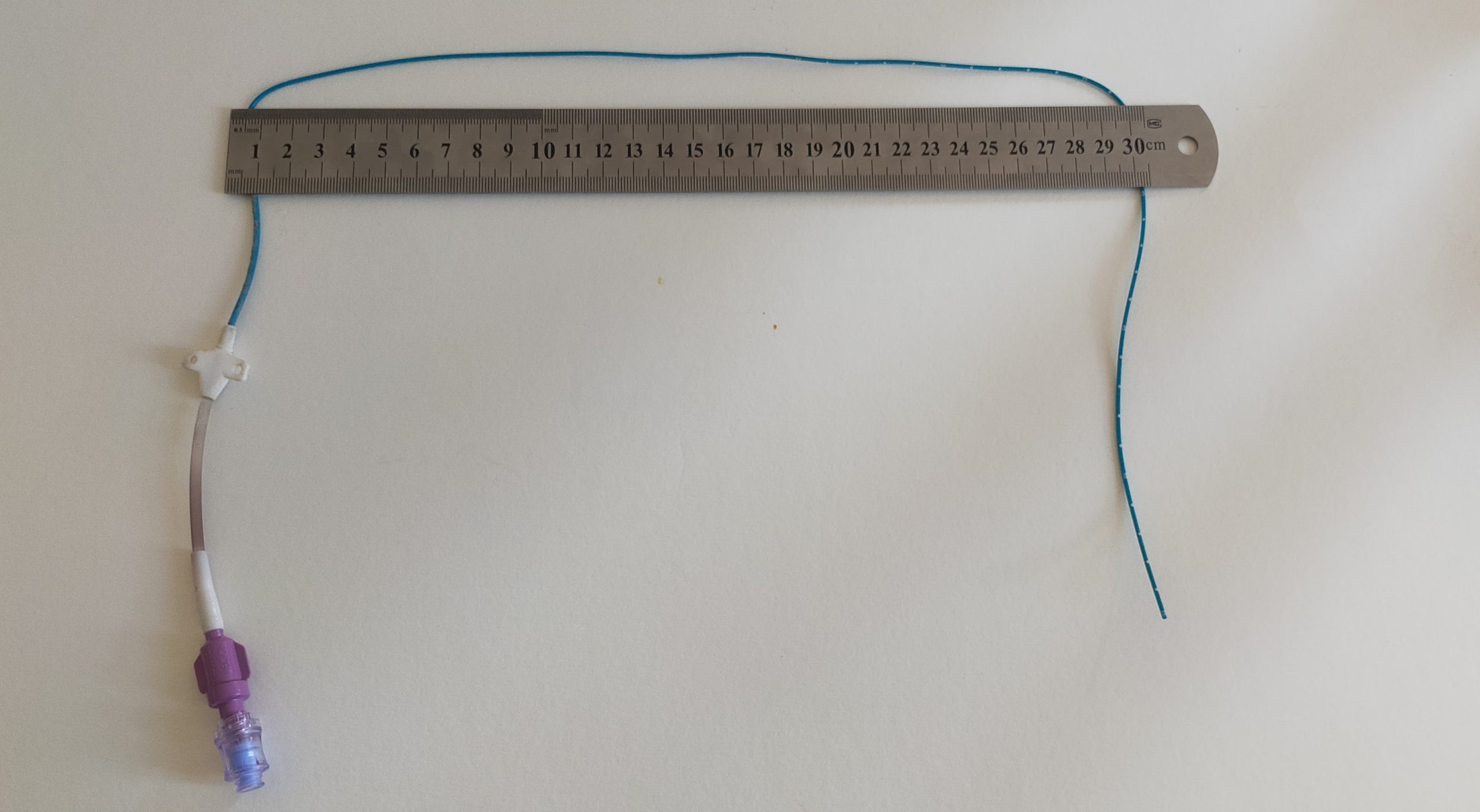
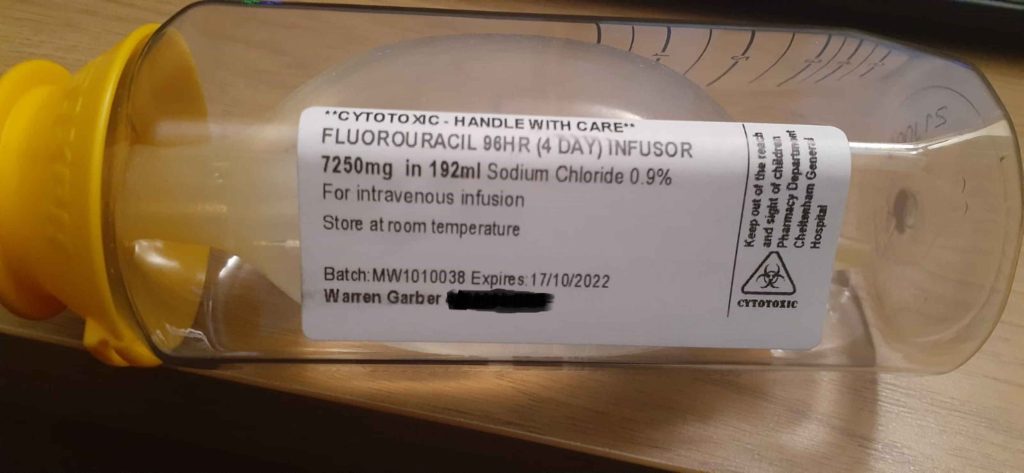
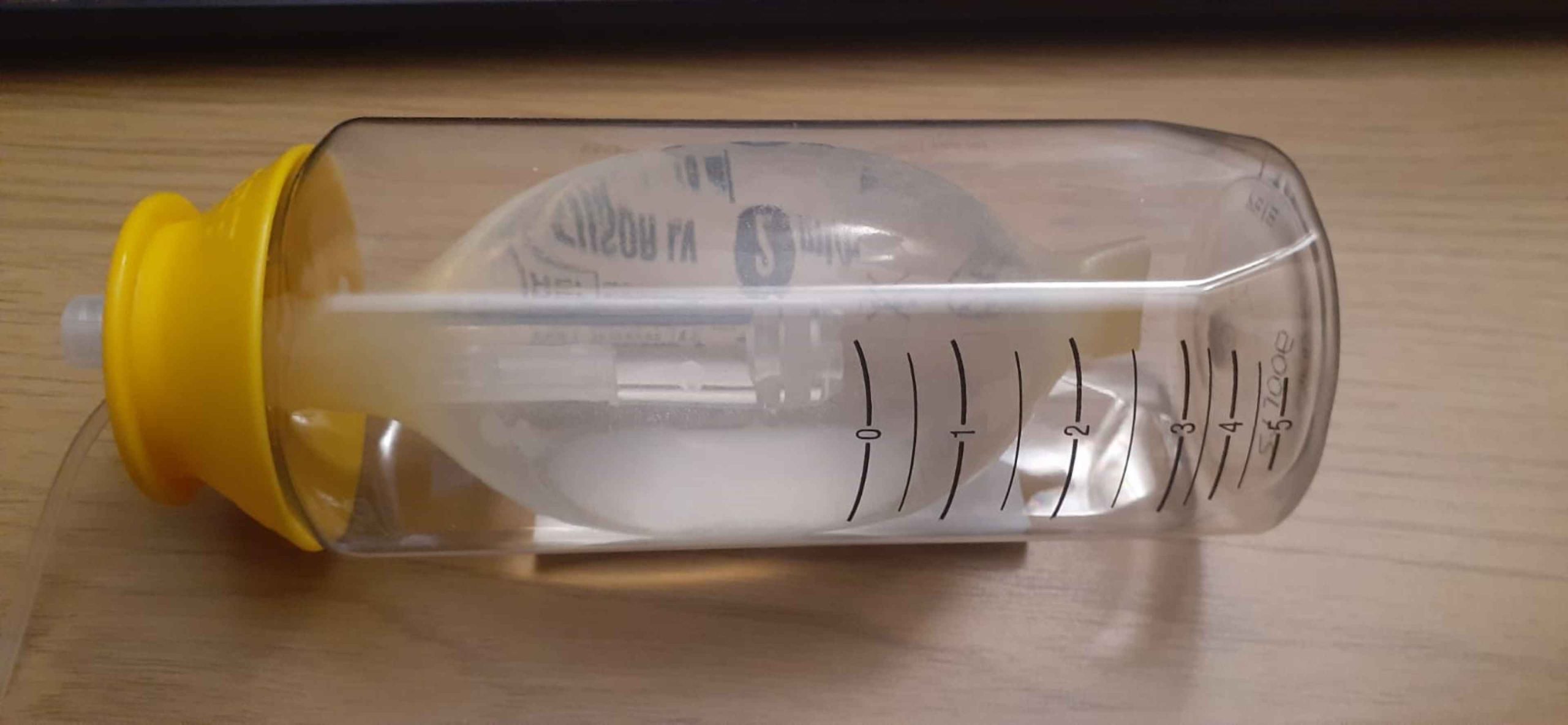
This is followed up by a good shot of Dexamethasone, which is a steroid. It’s used for many treatments, but in my case to help the body transition with the chemotherapy drugs. After that I get a dose of an anti-sickness medication and then finally hooked up to the Carboplatin chemo. This infusion takes around an hour.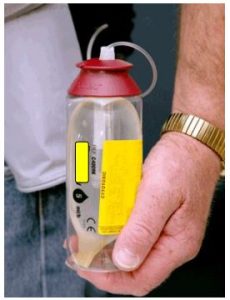 Kat puts it all together and places the Infusor into a small ‘bum bag’, which attaches to my belt. That’s me and the Infusor ‘married’ for a few days. I can’t disconnect it and must get used to it being there – including while sleeping, without of course, allowing the line to become tangled or disconnected.
Kat puts it all together and places the Infusor into a small ‘bum bag’, which attaches to my belt. That’s me and the Infusor ‘married’ for a few days. I can’t disconnect it and must get used to it being there – including while sleeping, without of course, allowing the line to become tangled or disconnected. It’s pretty amazing how we adapt to new things. In 60 odd years, I’ve never slept on my back – but immediately I find that wedging the Infuser behind my pillows, gives me enough play in the line that I can (almost) sleep comfortably.
It’s pretty amazing how we adapt to new things. In 60 odd years, I’ve never slept on my back – but immediately I find that wedging the Infuser behind my pillows, gives me enough play in the line that I can (almost) sleep comfortably.