43 – Trials or Tribulations
20th June 2023
Oh my word – I didn’t realise how long it’s been since I last wrote a blog post. A few kind people have contacted me separately to see if I’m still er, around.
And yep, I sure am around. Although the going has not been easy these past few months and I've found it a bit difficult in what to write.
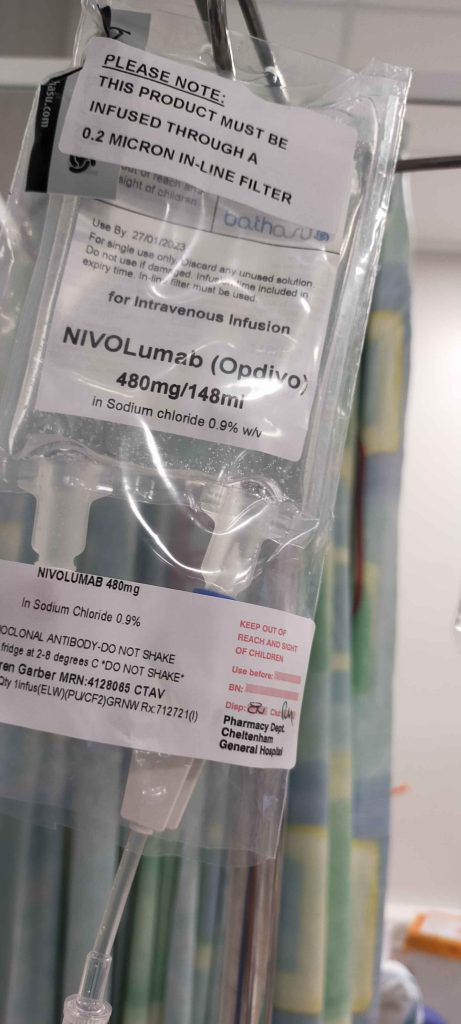
To catch up – I’ve now been through 8 cycles of immunotherapy and unfortunately CT scans are indicating that the treatment isn’t having any real effect on the tumours. In actual fact, the latest CT scan is showing that my tumours Tom, Dick and Harry are now coalescing together into one mass (or bulk soft tissue) as they like to call it.
Which isn’t particularly good news – although not all bad right now because still not showing any further spread, it’s seems I’m entering a new phase, entitled ‘Disease Progression’.
Well, to a simpleton like me, it’s all been progressing for the last 3 years. But to the medics it’s all expected, when the first two lines of treatment (Chemotherapy and then Immunotherapy), haven’t been successful.
So right now, we’re at a bit of a crossroads in terms of what’s next.
There is the possibility of joining a clinical trial of some new treatments under test conditions. I’ll be finding out more about this over the next 2 or 3 weeks. From prior experience looking at trials, there are a number of known unknowns and indeed unknown unknowns. So quite a lot to consider before leaving the care of my dear Dr Grant and entrusting others, most likely at a hospital in London.
The other – and seemingly only choice, is a 3rd line chemotherapy with Docetaxel, which is a pretty aggressive chemo drug. Scraping the bottom of the test-tube, kind of thing I reckon😉
But at least this would be with Dr Grant and his superb team here in Gloucestershire
Anyway, I hope to find out more soon about both and then will have to decide on a route.
In the meantime, now that Tom, Dick and Harry and joining together into one mass (so to speak), I’ve been giving thought to a new name for it.
After just a few nanoseconds of brain strain, I’ve decided on Big Dick as the new name for my right-lung soft tissue thingy.
Absolutely not to be confused with any other soft-tissue thingies.
Make a note people 😊
Until next time…
Stay safe
Woz






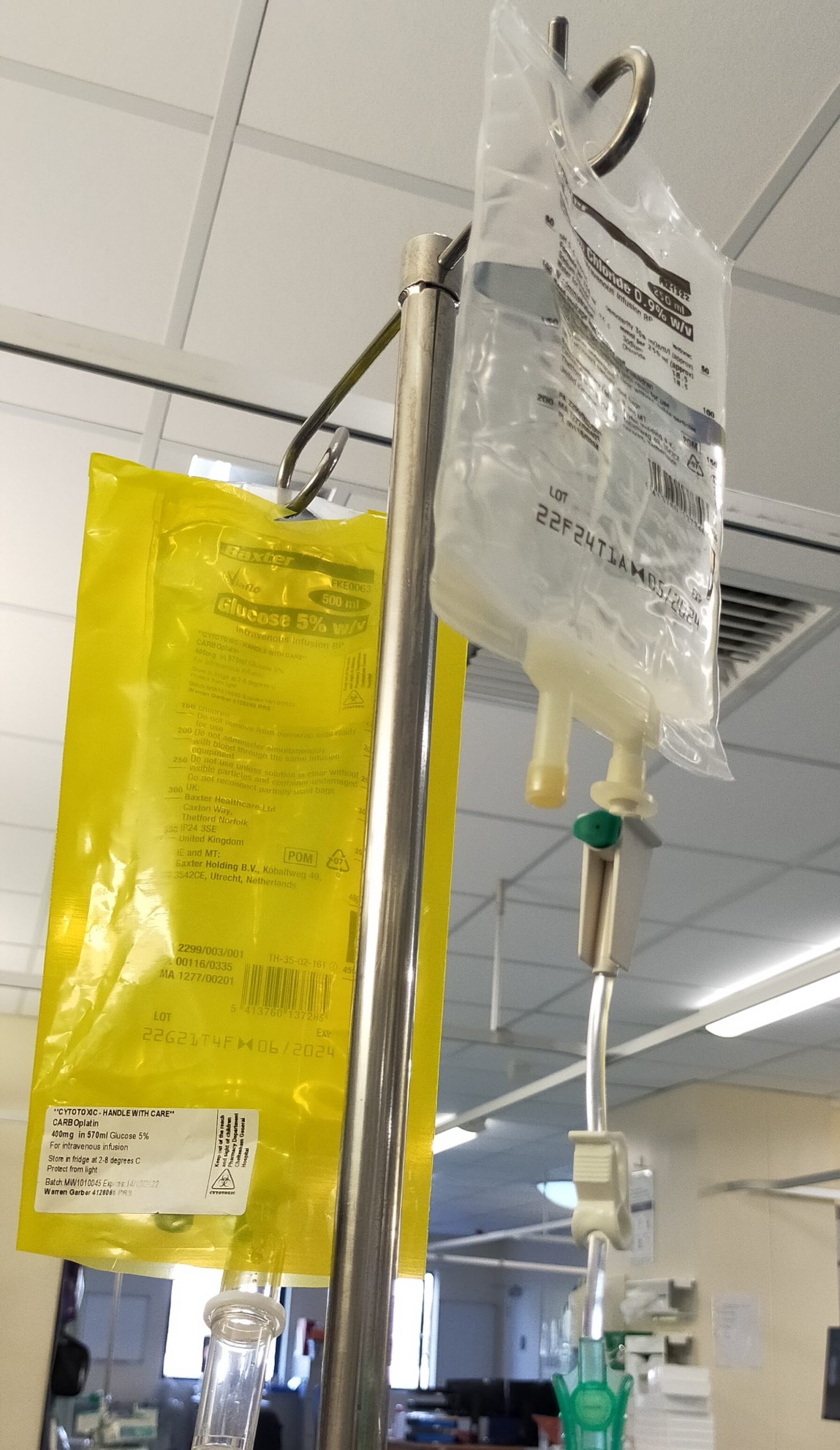

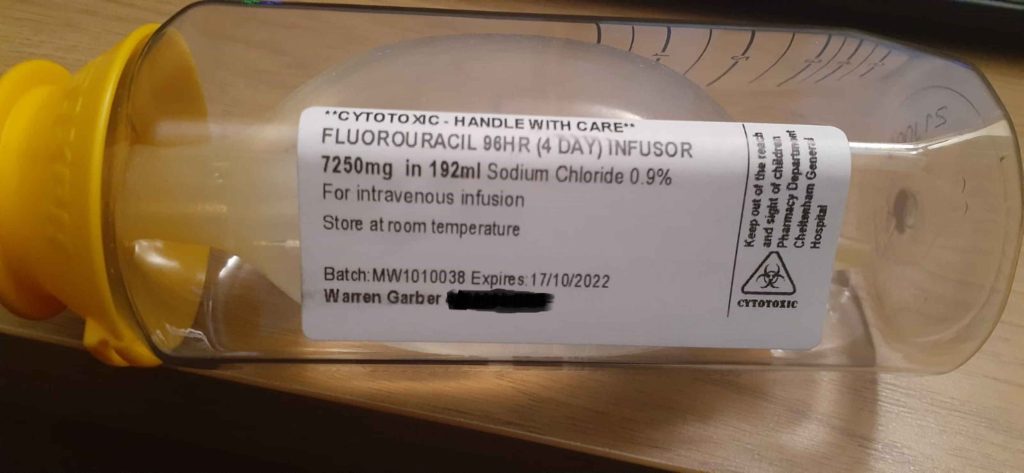
















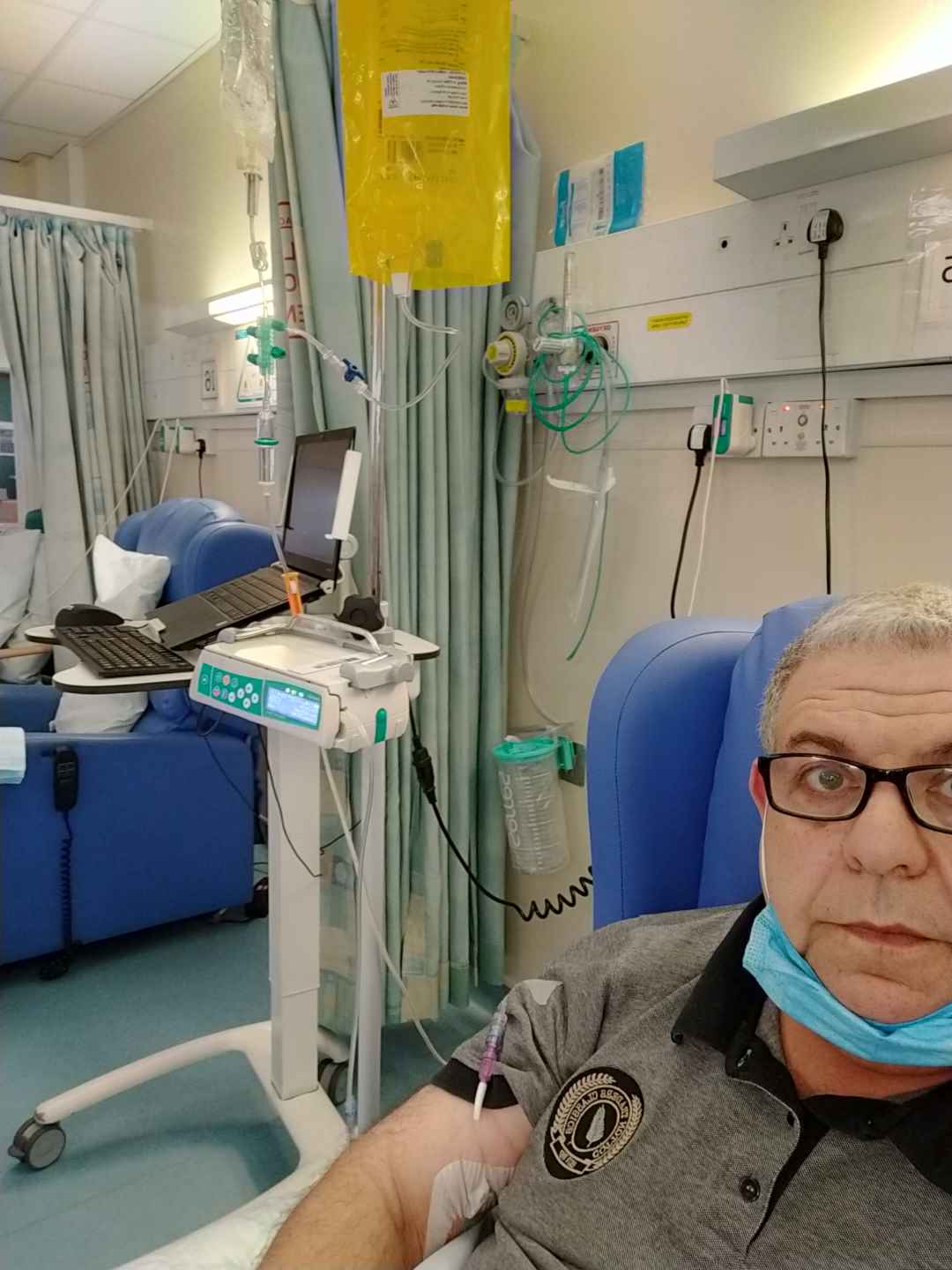
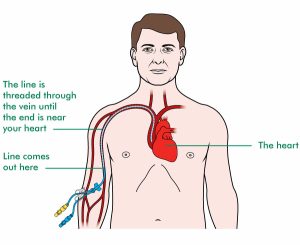
 This is followed up by a good shot of Dexamethasone, which is a steroid. It’s used for many treatments, but in my case to help the body transition with the chemotherapy drugs. After that I get a dose of an anti-sickness medication and then finally hooked up to the Carboplatin chemo. This infusion takes around an hour.
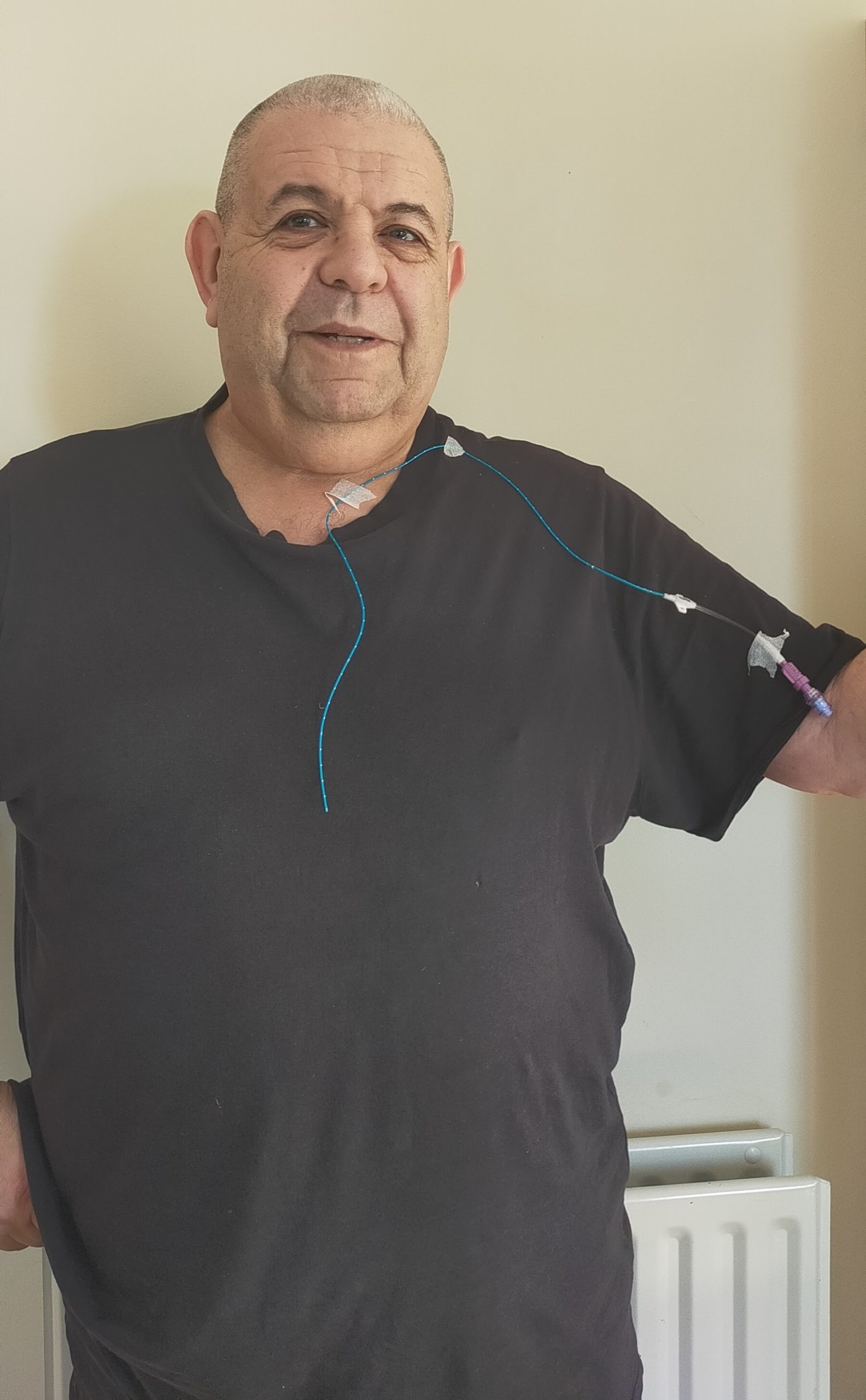
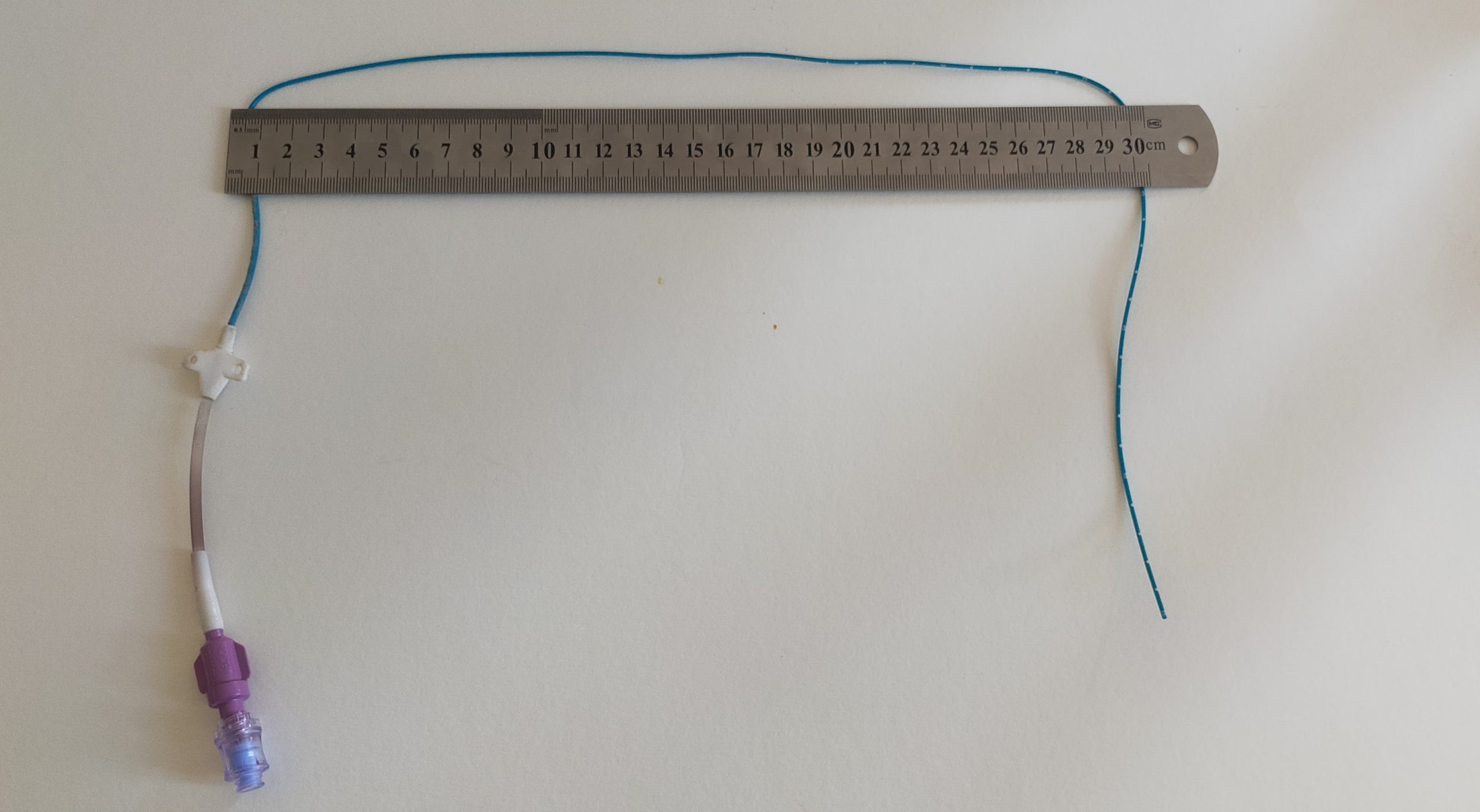
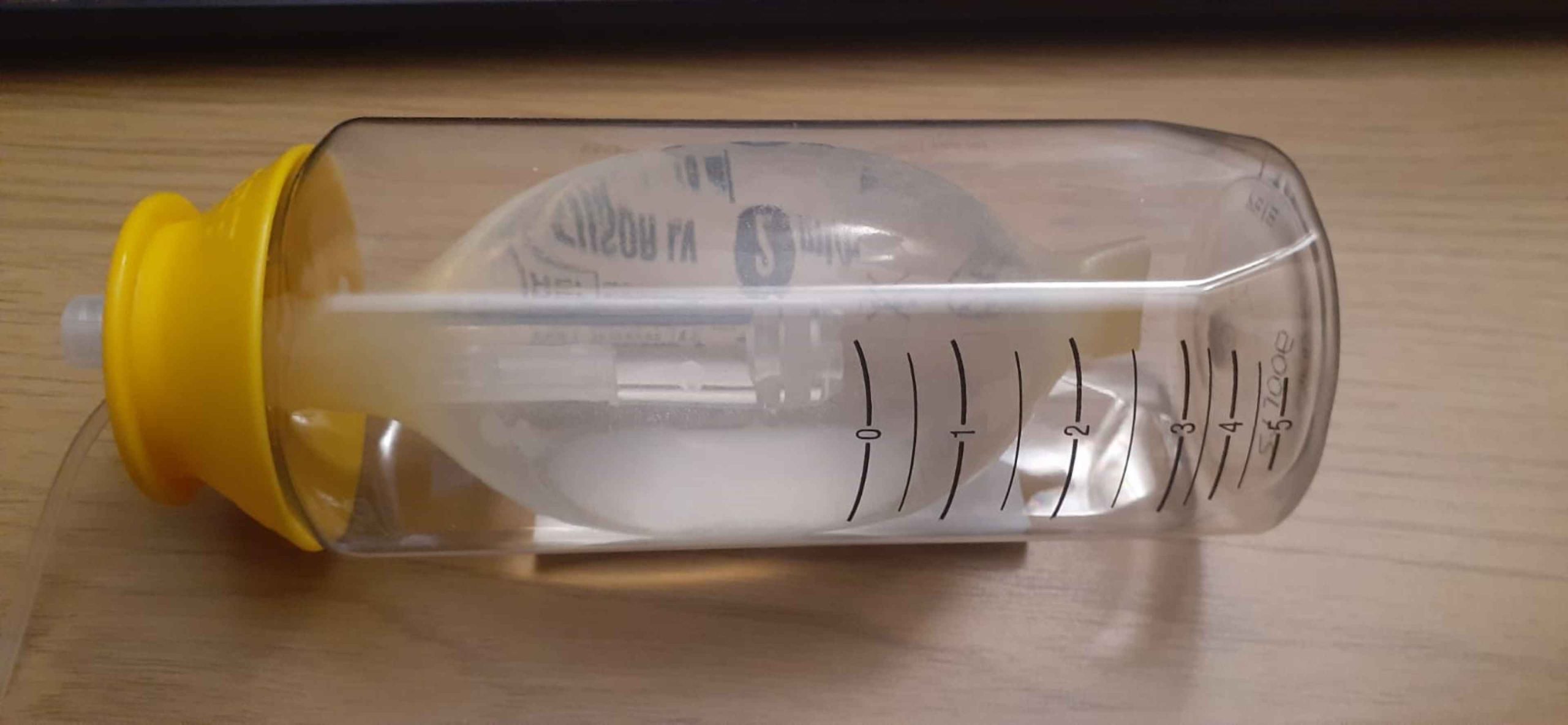
This is followed up by a good shot of Dexamethasone, which is a steroid. It’s used for many treatments, but in my case to help the body transition with the chemotherapy drugs. After that I get a dose of an anti-sickness medication and then finally hooked up to the Carboplatin chemo. This infusion takes around an hour.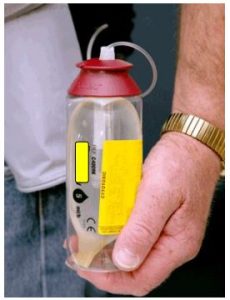 Kat puts it all together and places the Infusor into a small ‘bum bag’, which attaches to my belt. That’s me and the Infusor ‘married’ for a few days. I can’t disconnect it and must get used to it being there – including while sleeping, without of course, allowing the line to become tangled or disconnected.
Kat puts it all together and places the Infusor into a small ‘bum bag’, which attaches to my belt. That’s me and the Infusor ‘married’ for a few days. I can’t disconnect it and must get used to it being there – including while sleeping, without of course, allowing the line to become tangled or disconnected. It’s pretty amazing how we adapt to new things. In 60 odd years, I’ve never slept on my back – but immediately I find that wedging the Infuser behind my pillows, gives me enough play in the line that I can (almost) sleep comfortably.
It’s pretty amazing how we adapt to new things. In 60 odd years, I’ve never slept on my back – but immediately I find that wedging the Infuser behind my pillows, gives me enough play in the line that I can (almost) sleep comfortably.