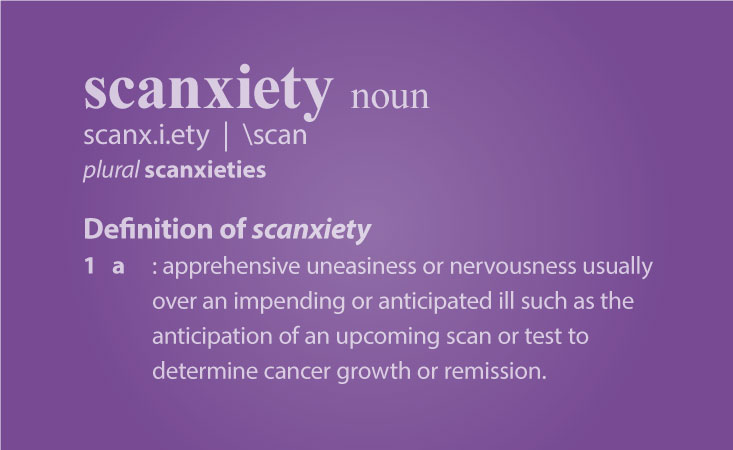
40 – Cancer Scan Anxiety and Scanxiety
10 November 2022
I’d touched on the scan and especially reporting delays in my last post. And it appears to becoming an issue countrywide. One cancer patient I’m in touch with, was still waiting for his scan report, almost 3 months after the scan – and almost in time for his next scan!
So, what on earth is going on?
The system seems to be that once a patient has a scan, the images are interpreted by a Radiologist who then writes a report and forwards said report to the specialist doctor. The doctor then considers the report and decides on the best treatment for the patient.
All good and the system worked pretty well, until what appears to be a backlog due to a combination of Covid delays and lack of trained personnel.
I did a bit of delving, but didn’t get very far with my local NHS Trust. Certainly not without making a ‘Freedom of Information’ request. And I don’t have the energy or inclination, for all of that.
But, talking to a doctor recently, it’s clear that scan reporting is likely to be an ongoing issue for the foreseeable future.
As he put it to me ‘They can keep producing scanning units every day, but it takes around 10 years to fully train a Radiologist to interpret scans professionally’.
In a way then, my 3.5 weeks wait for the results wasn’t a long time in the big scheme of things, but an eternity in terms of anxiety, not knowing how things are.
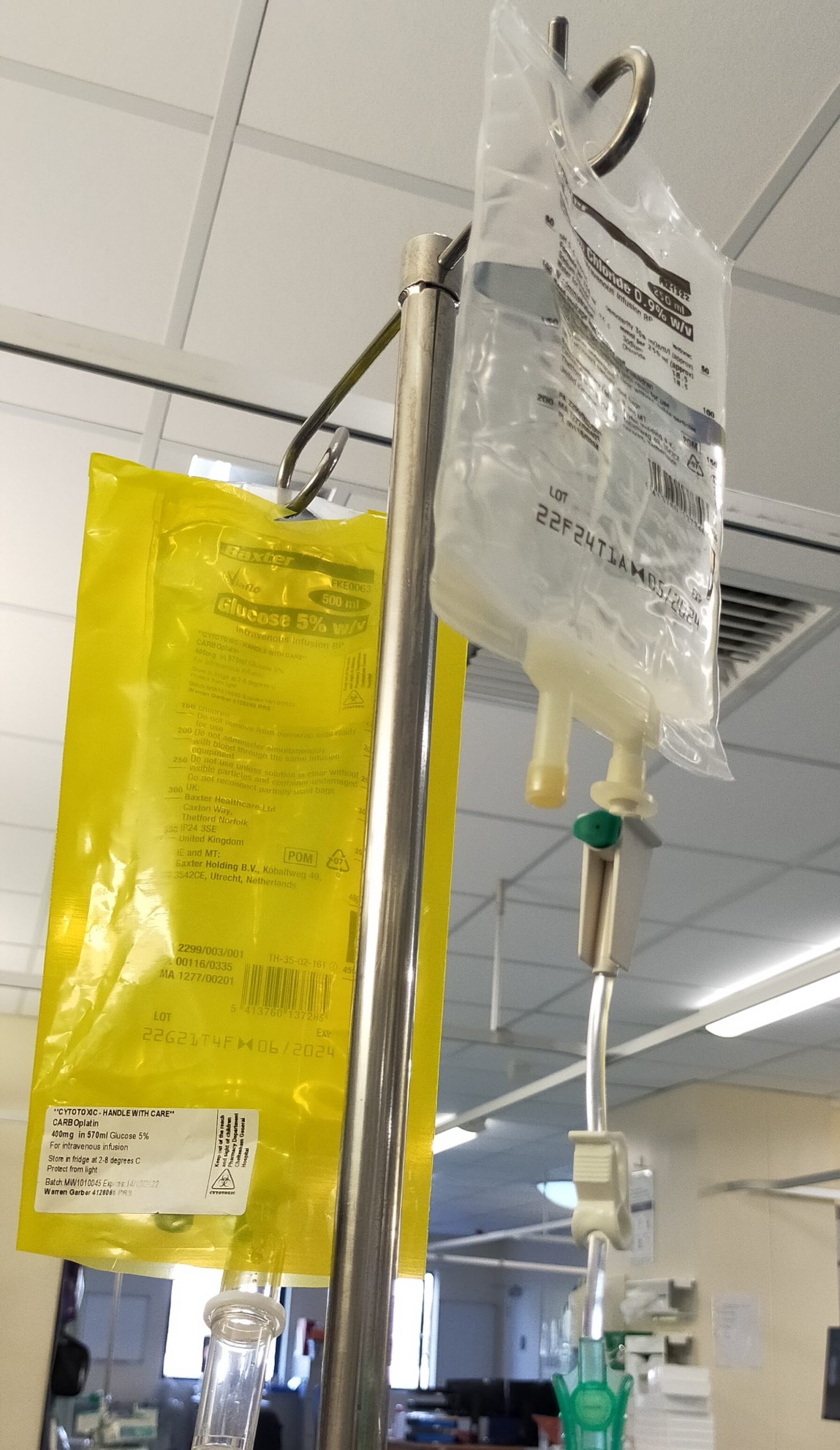
And unfortunately, it wasn’t the news I was hoping for. The 18 weeks of chemotherapy didn’t shrink any of the tumours, and in fact the largest (Tom) had increased in size by some 50% from 40mm to almost 60mm. Dr Grant was also very disappointed by the results.
If there are any positives to take from this, no further spread has been detected. Whether that’s due to the chemo or just natural, is impossible to tell right now, but suffice to say that because the first-line (chemo) treatment was unsuccessful, then some careful consideration had to be given to the next steps.
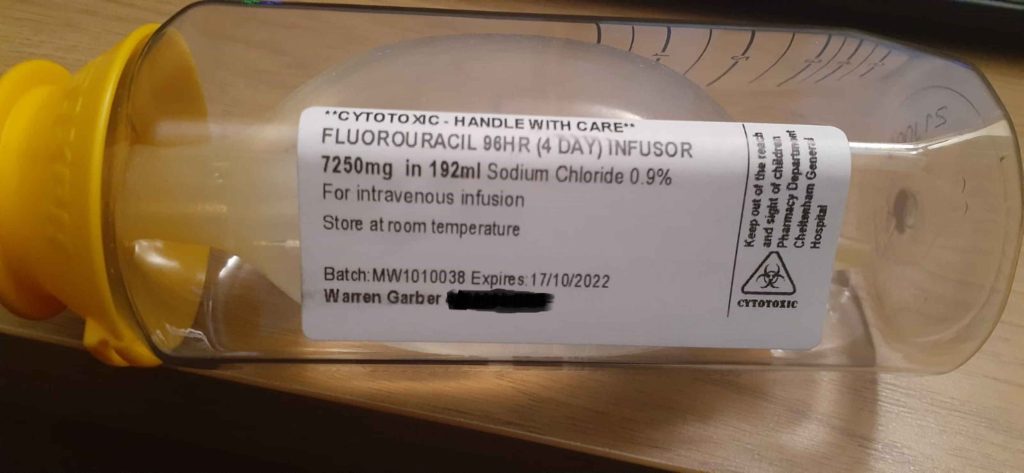
These ranged from pause treatment for a few months and then scan again; use a different type of chemo or start with a course of Immunotherapy. We discussed the options and agreed to run with the latter. So later this month, I’ll be back for bi-weekly infusions of a drug named Nivolumab.
I begin next week 16th November – with preliminary checks and tests and then my first infusion is scheduled for 21st November and then every 2 weeks after that. I guess quite a bit depends on how I react to the treatment.
Dr Grant tells me that I have to be aware of anything ending in ‘itis’ (inflammation) i.e. dermatitis, colitis, hepatitis etc. This is because the drug alters the body’s own immune system and while generally well tolerated, it can have quite unpredictable and serious effects
Anyway, I’m sure I’ll learn a lot more in the next few weeks – if nothing else I’ll have lots more material for my blog 😊
So, all being well, I’ll write an update after my second cycle in December. Until then, wherever in the world you are – take care x