50 – Four years on and living to tell the tale
27 March 2024
Wow! This time it’s been three months since my last blog post – and the main reason is…
No excuse really!
It’s just coming on to 4 years since my initial cancer diagnosis, back in those crazy days of April 2020, when the Covid pandemic was just unfolding.
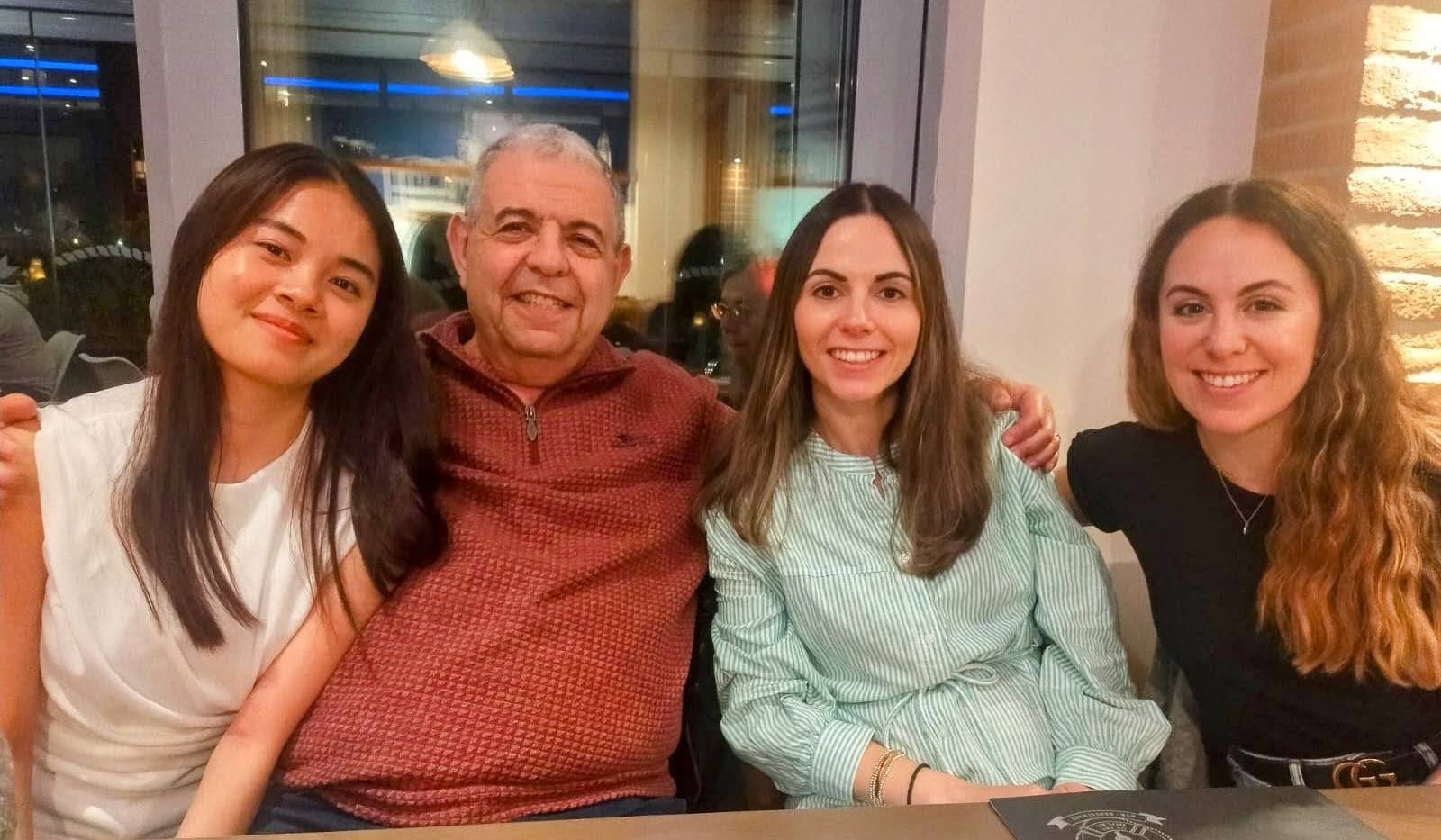
As a close family, we’ve been through a fair share of ups and downs. I’ve surpassed most prognoses, which in fairness are at best an assessment on the success(es) of treatment(s) and what generally happens to patients of similar state of health.
It was nearly 2 years ago that things weren’t looking so good and this was the first time Samros and me were introduced to another of the NHS protocols that we don’t know about – until we need to know about them. There we were sitting with my GP in her surgery in mid-2022, discussing end-of-life (EOL) care. There were options open to us about the how, what and where things should happen.
I won’t go into the fine details, but one thing that did happen as part of the protocol is to issue me with a box of EOL drugs, to keep at home and that remains sealed until the medics need to use them. The NHS euphemistically calls it a ‘Just in Case’ box.
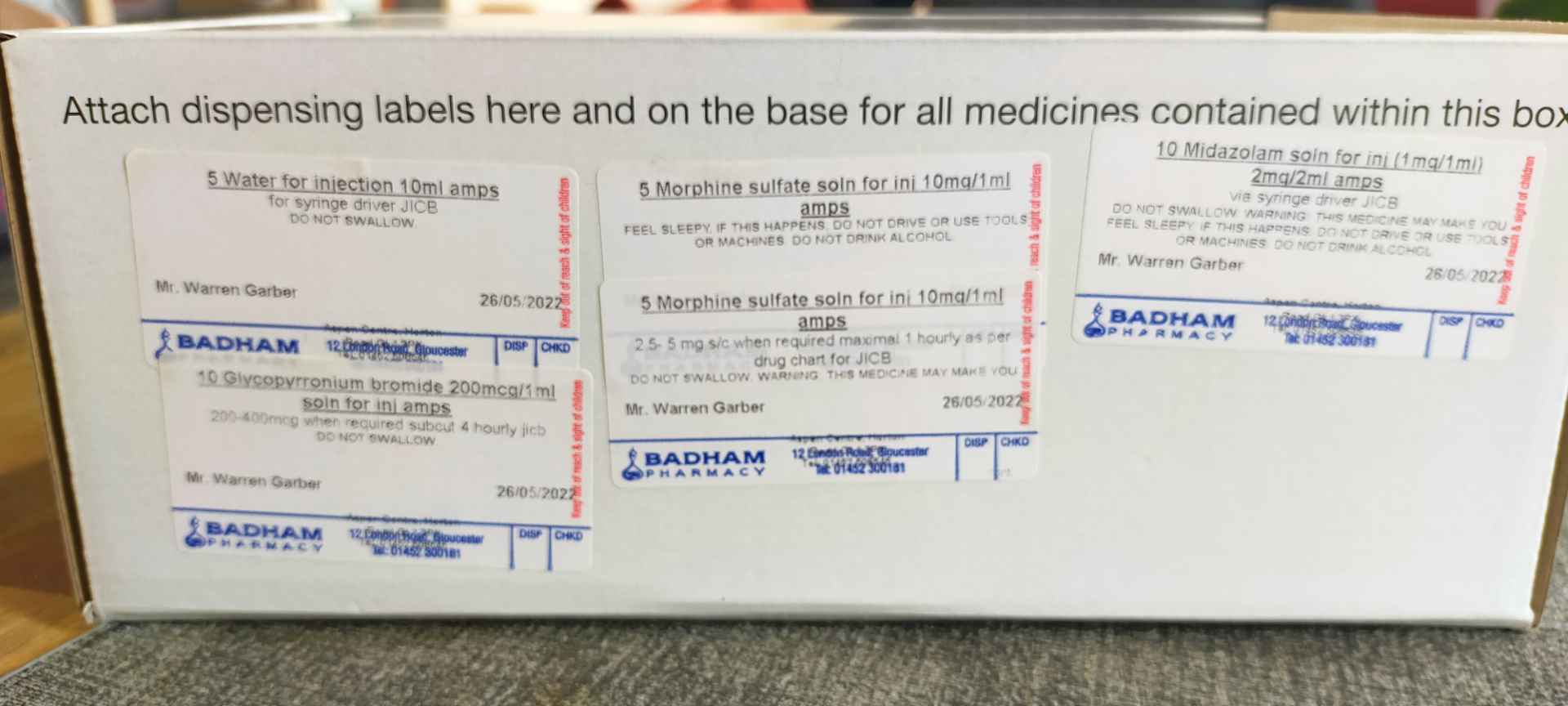
So you might be able to imagine our joy when I returned the box to the pharmacy last week, because the EOL drugs have expired their use by date.
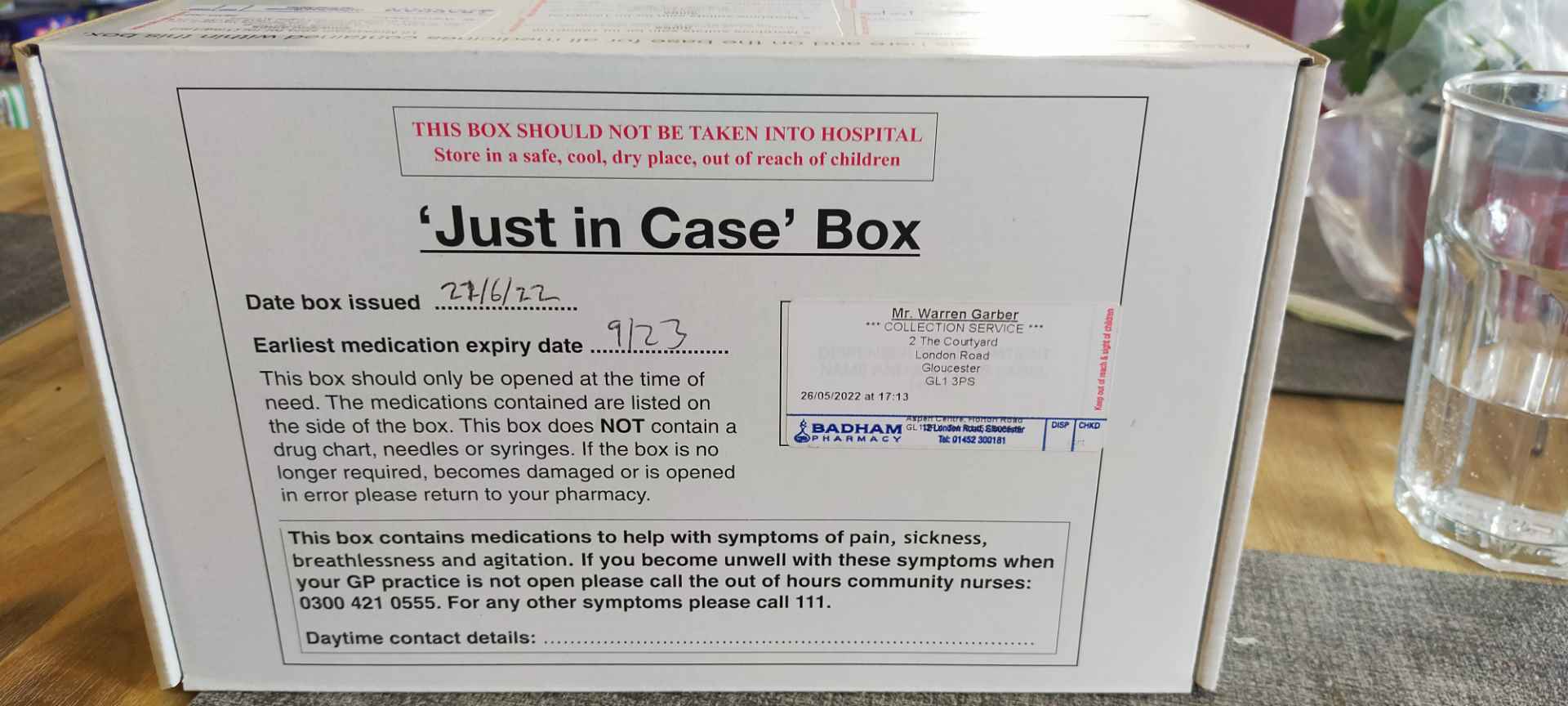
It’s a great feeling to outlive the end-of-life drugs and if I say so myself – I love the irony of this. And of course, the smiles I received from the pharmacy staff too.
Medically, our National Health Service continues to excel itself in terms of my care. Since I last wrote – I had a CT scan in January which is still showing no real development of my right-lung tumours – although there is some growth and I’m still being monitored by both the ever-wonderful Dr Grant and also by The Royal Marsden. It don’t get much better really.
The tumour growth I mentioned is, we believe, small but significant enough to affect a nerve somewhere that’s troubled me on and off for the 2-3 years. But it’s now more constant and normal painkillers of various flavours aren’t doing the trick any more.
So, I’m back on morphine and this will most likely continue for the foreseeable future.
I have a slow-release morphine capsule – which is taken orally morning at night time.

It’s a fairly low dose, which dulls, rather than completely eradicates the pain. The slow-release action spreads the effect over around 10 hours. This is in contrast to ‘normal’ morphine which gives a more immediate relief, but over a shorter period.
I prefer this low dose, so it doesn’t affect my driving and generally I hope not to become too addicted or dependent in the future. But probably will at some point.
Along with this – I did have lung function tests and a follow-up with a respiratory consultant, to discuss my breathlessness in general and my (clinical trial) damaged left lung in particular.
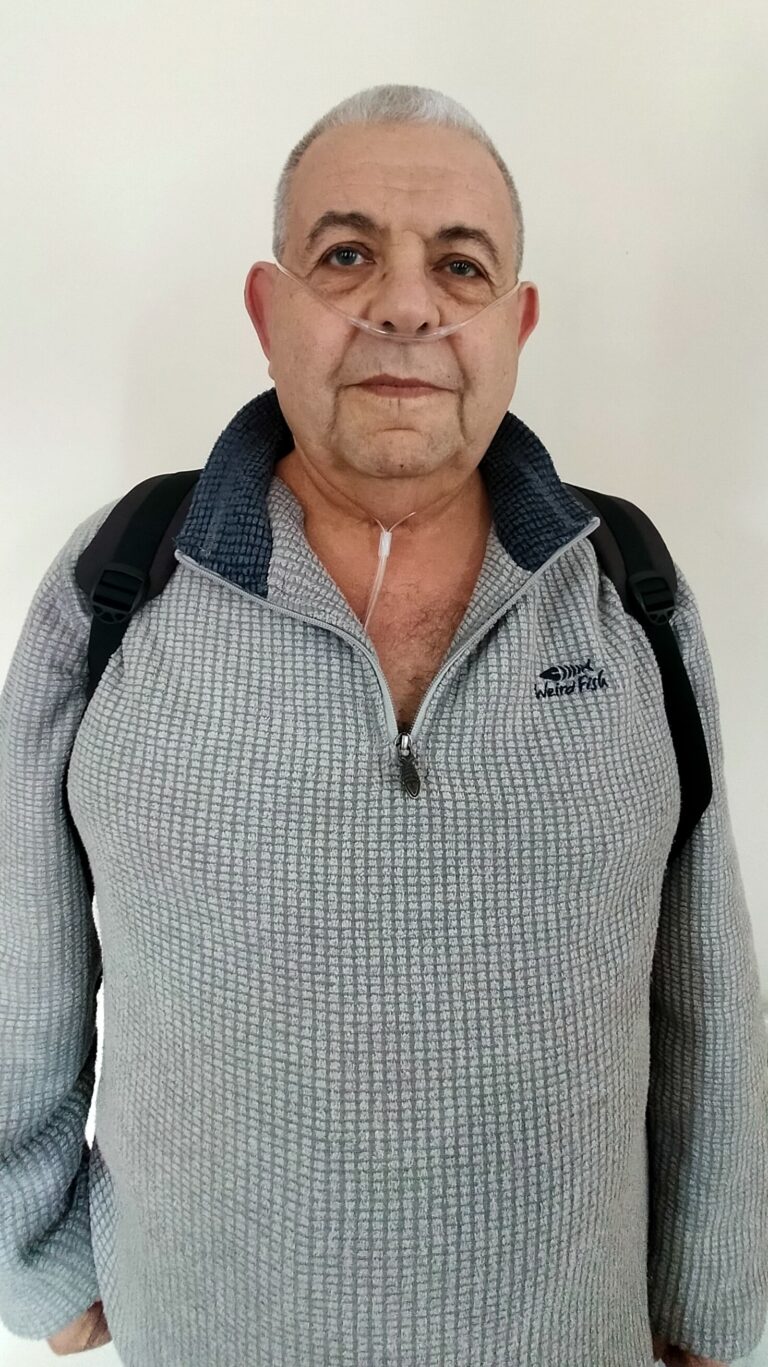
While the inflammation has subsided in the main – I’m still on supplemental oxygen, although I do try short, level walks without it. Again, this is because I hope not to be dependent – and also for me, I’ve become quite self-aware of the plastic tubes (cannula) that go in my nose.
It could be argued I’m not a pretty sight at the best of times – unfortunately a nose cannula does absolutely nothing to improve that 😉
Anyway – for the time being I’m still on external oxygen when required and I’ll have some more tests and further evaluation / consultation around mid-year. That’s when I should get to know whether this will be a permanent accessory, or not.
And if all of that isn’t enough, we’re finally getting somewhere with the falling-down/ dizzy spells stuff. I had a meeting with a consultant physician at Gloucester Royal Hospital, Syncope dept.
I think Syncope is a much better term for fainting/falling down. Doesn’t sound so ‘old people / silly old git’.
The tests began with blood pressure readings taken laying down and standing up. My laying down reading was 135/59 mmHg, but after 5 minutes of standing up, the reading was just 55/25 mmHg. Not good at all – but nothing new to me as I’d been monitoring my BP with a home test kits pretty much daily.
This has been officially diagnosed as Orthostatic Hypotension, which simply means low blood pressure, when standing – especially from a prone position.
The interesting thing is what causes the significant drop. It’s known as autonomic failure or autonomic dysfunction.
So, as I understand it – our autonomic function(s) are those things that the brain controls and happens without us having to think about it – examples being what makes our heart beat, eye blinking and so on.
Now – when we stand up from a sitting or laying position – our autonomic system is supposed to counteract the natural tendency of blood falling to our legs by gravity. It does this by restricting the blood vessels in our legs and increasing our heartbeat – so that oxygen-containing blood is sent back up to our brain.
When this doesn’t happen – as in my condition, then the brain can sense the lack of oxygen and quickly shuts down functions that aren’t required at that moment. Legs aren’t really required, so the muscles don’t function and this usually results in the fainting / momentary loss of consciousness episodes that occur.
Many people might experience a slight feeling of dizziness when standing quickly, but their body counteracts things quicker than mine is capable of, so they don’t fall down.
These also a discussion that my lower oxygen levels due to damage now to both lungs, is possibly exacerbating the blood oxygen / brain function issue. Well, that’s my excuse for many things that I forget now!

So, apart from the right-lung tumours and radiotherapy scarring, my left-lung damage do to severe pneumonitis and my autonomic disfunction thingy – I’m doing okay!!
And this is what people are saying to me – ‘you look well Woz’. Even my GP and Oncologists say this.
So it can’t be all that bad.It even makes for some moderately interesting subjects to write about 😊
Until next time…
Woz






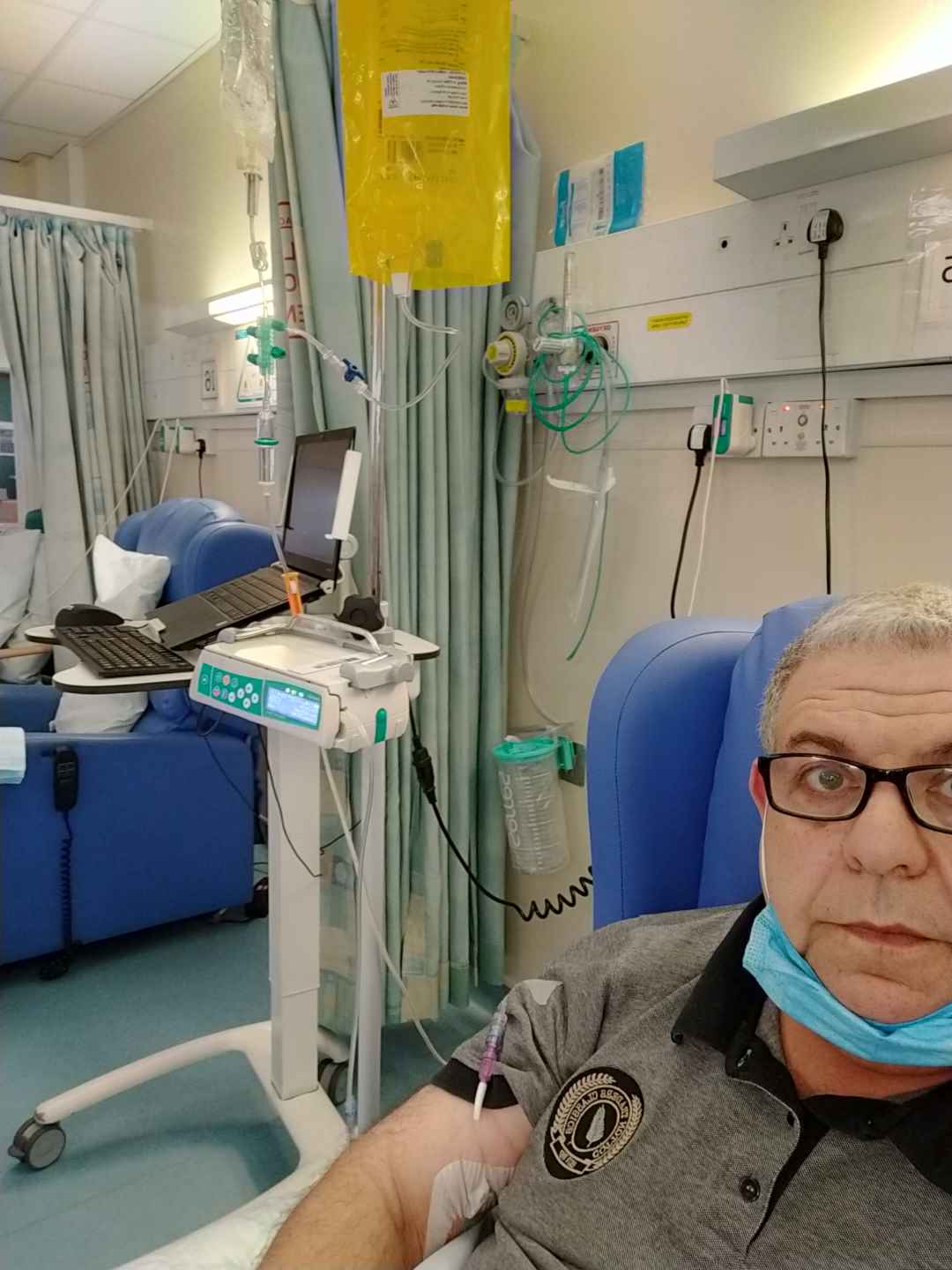
 This is followed up by a good shot of Dexamethasone, which is a steroid. It’s used for many treatments, but in my case to help the body transition with the chemotherapy drugs. After that I get a dose of an anti-sickness medication and then finally hooked up to the Carboplatin chemo. This infusion takes around an hour.
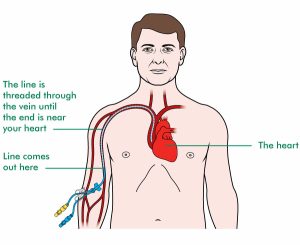
This is followed up by a good shot of Dexamethasone, which is a steroid. It’s used for many treatments, but in my case to help the body transition with the chemotherapy drugs. After that I get a dose of an anti-sickness medication and then finally hooked up to the Carboplatin chemo. This infusion takes around an hour.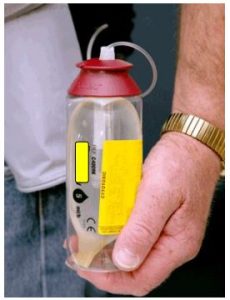 Kat puts it all together and places the Infusor into a small ‘bum bag’, which attaches to my belt. That’s me and the Infusor ‘married’ for a few days. I can’t disconnect it and must get used to it being there – including while sleeping, without of course, allowing the line to become tangled or disconnected.
Kat puts it all together and places the Infusor into a small ‘bum bag’, which attaches to my belt. That’s me and the Infusor ‘married’ for a few days. I can’t disconnect it and must get used to it being there – including while sleeping, without of course, allowing the line to become tangled or disconnected. It’s pretty amazing how we adapt to new things. In 60 odd years, I’ve never slept on my back – but immediately I find that wedging the Infuser behind my pillows, gives me enough play in the line that I can (almost) sleep comfortably.
It’s pretty amazing how we adapt to new things. In 60 odd years, I’ve never slept on my back – but immediately I find that wedging the Infuser behind my pillows, gives me enough play in the line that I can (almost) sleep comfortably.